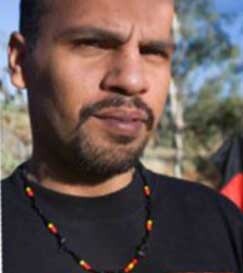
Confidentiality & Privacy - Troy's Story
Troy is an Aboriginal man from Perth who was concerned about his sexual health and took the opportunity to seek tests at a rural clinic whilst visiting friends.
Initial consultation
In the first consultation the Health Care Professional (HCP) undertook a series of tests and provided Troy with reassurance that sexual health conditions are treatable if identified early and that if the tests were positive, he would be assisted to get treatment. This conversation helped Troy feel more relaxed and build trust.
He explained that it would be ideal if Troy could come back to the clinic to receive the pathology results whether they were positive or negative which could take up to two weeks. Troy advised he wouldn’t come back to the clinic as he was planning to go North in a couple of days. Given Troy’s mobility, the HCP asked for more contact details.
Troy told the HCP that when he lived in Perth, he stayed with his Aunty who lived at the residential address provided on the Client Form. However, when he was away, he often checked in with his sister who kept him up to date with things. Troy advised his preference was for the HCP to try contacting him on his mobile number or trying his sister’s mobile as she was able to get word to him. The HCP reassured Troy that he would only ask his sister to get Troy to call him to contact his HCP for his medical test results and noted in Troy’s file that no communication be provided to the residential address on the client form.
The HCP explained that if Troy did receive a positive test the Public Health Unit would be automatically notified and that he will be required to provide a list of people he had sexual contact with to ensure they were advised to get tested. The HCP explained that he could work with Troy to identify who his contacts were, or Troy could choose to have a person in the Public Health Unit work with him. Troy was reassured that the Public Health Unit would protect his confidentiality. Troy said he felt comfortable working with the HCP to compile the list. However, Troy said that as his recent contacts were casual, and he couldn’t recall their names, that he will check in with his mate who knew their names.
The HCP received pathology results that Troy is HIV positive
The HCP tried unsuccessfully to phone Troy on his mobile. He then phoned Troy’s sister who said she would pass on the message to Troy to phone the HCP. Troy called the HCP a few days later from a remote community clinic. The HCP advised Troy of the diagnosis and with Troy’s permission made arrangements for the Aboriginal Health Worker to sit with him while he explained the recommended treatment and how to access it as well as where he could get support.
Troy provided the HCP with a list of the close contacts as discussed. Most contacts had a first name only, approximate age, a brief description, a town of where he thought they came from, and in some cases a description of the car they drove. The HCP assured him this was a great start.
Troy was told that he could advise the contacts himself or he could ask the HCP or the Public Health Unit to advise the contacts. Troy’s preference was for the Public Health Unit to follow up as it was more likely to be able to find them quickly. Troy was reminded that the Public Health Unit would protect his confidentiality.
The HCP provided this information to the Public Health Unit which in turn engaged with an Aboriginal Community Controlled Health Organisation (ACCHO) that agreed to assist. Information pertaining to Troy as the index person was not provided to the ACCHO.
Page last updated October 2022